Understanding Diagnosis and Assessments
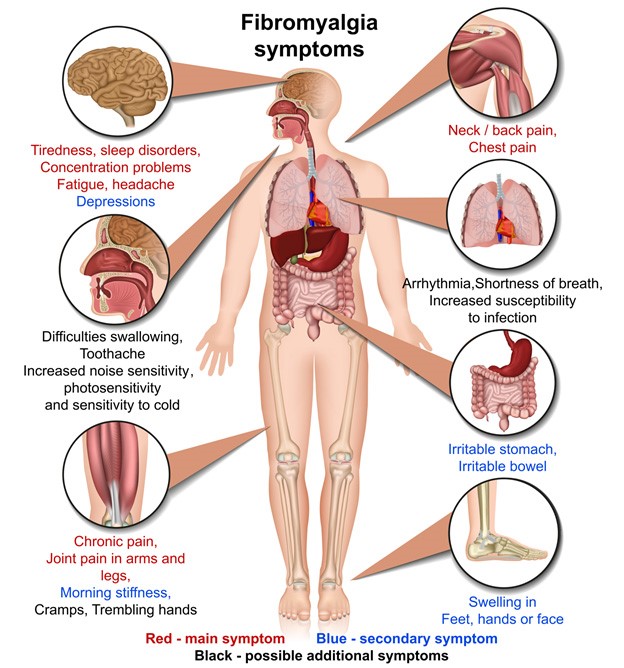
Fibromyalgia (FMS) is a complex multisystem physical disorder, a primary chronic pain condition (classified in the WHO International Classification of Diseases: ICD-11 Version: 2019).
The ongoing widespread body pain is complex. It varies in different people but can involve the muscles, ligaments, tendons and surrounding structures without any obvious tissue damage.
Diagnostic Process
Fibromyalgia is diagnosed with a careful history, a physical examination, as well as a symptom questionnaire based on the diagnostic criteria, and appropriate blood tests to exclude other or diagnose coexisting conditions.
1. History
- Take a thorough history, looking for widespread pain over time.
- Onset – abrupt or gradual, or if related to an event or illness
- Course – stable, improving, or worsening
- Duration and daily pattern (pain often has mixed inflammatory and mechanical features, often with neuropathic descriptors).
- Factors that alleviate or exacerbate symptoms
- Impact on daily life – ability to work, socialise, participate in family activities
- Accommodations that patient and/or family has made to adjust to pain/fatigue symptoms
- Tests to exclude any other disorders that fully explain the symptoms.
Useful Survey Questionnaires
- Fibromyalgia Survey Questionnaire (Hauser et al, 2012) to quantify the major symptoms of the syndrome.
- Fibromyalgia Canadian Multisystem Questionnaire, to identify the range of the symptoms and domains
- Bell’s Functionality Score, to assess severity of symptoms
2. Examination
- Physical examination to cover musculoskeletal and neurological changes: muscle weakness, neurological signs and/or other physical symptoms that may indicate any overlapping condition.
- Check for lymphadenopathy, thyroid disease, cardiac or pulmonary disease, joint or connective tissue disease
- Look for diffuse tenderness in soft tissues
- Do lying and standing blood pressures
- During assessment list any treatable/management areas e.g.
- Sleep disorders
- Underlying arthritic inflammatory conditions
- Depression or anxiety
- Gut issues
- Other primary pain conditions
3. Investigations
– Routine blood tests to exclude other conditions and/or comorbidities
- FBC, CRP, ferritin, creatinine
- Electrolytes, renal and liver function, calcium, magnesium
- Fasting blood glucose and insulin
- Thyroid function and antibodies (TSH, T3, T4)
- B12, Folate, Vitamin D
- Iron Studies
- Urinalysis
Other tests as clinically indicated:
- Inflammatory muscle disease, creatinine kinase
- Infection markers for recent or ongoing infections; viral, consider EBV, cytomegalovirus, HIV, Q Fever.
- Immunoglobulins, antinuclear antibodies, rheumatoid titres
- Coeliac antibodies
- Fasting am cortisol and DHEA
4. Referral to Specialists
Only required when there is significant uncertainty about the diagnosis, or predominant symptoms are suggestive of underlying or overlapping diagnoses and for specific areas of management
5. Further Ongoing Assessments
Further ongoing assessments will guide Clinical Management and allied health referrals.
What you can do
- Learn about Fibromyalgia, the types of pain and the treatments available
- Pace yourself
- Use the ‘one at a time’, ‘start low, go slow’method when trying new treatments and interventions
- Keep good records of symptoms and treatment outcomes using a diary or app
- Provide accurate feedback and good communication to your providers
- Keep to your action plan and/or care plan
- Maintain support networks with family and friends.