Comprehensive Assessment

In General Practice, Fibromyalgia can be diagnosed with a careful history, using a validated practice self-assessment tool based on the diagnostic criteria, a thorough physical examination, and appropriate blood tests to diagnose other overlapping and/or coexisting conditions.
1. History
Take a thorough history, looking for widespread pain over time.
- Onset – abrupt or gradual, or if related to an event or illness
- Course – stable, improving, or worsening
- Duration and daily pattern (pain often has mixed inflammatory and mechanical features, often with neuropathic descriptors)
- Factors that alleviate or exacerbate symptoms
- Impact on daily life – ability to work, socialise, participate in family activities
- Accommodations that patient and/or family has made to adapt to pain/fatigue symptoms
- To quantitate the various symptoms of the syndrome use the Fibromyalgia Questionnaire (Hauser et al, 2012)
- The 2011 Fibromyalgia Michigan Body Map diagnostic tool is useful to determine the degree of Fibromyalgia or central sensitisation
- To identify the range of symptoms and domains use the Fibromyalgia Canadian Consensus Questionnaire
- Exclude any other disorders that fully explain the symptoms.
2. Physical Examination
a. Perform a full musculoskeletal and neurological examination looking for muscle weakness, focal neurological signs and/or to identify other overlapping conditions
- Check for lymphadenopathy, thyroid disease, cardiac or pulmonary disease, joint or connective tissue disease
- Look for diffuse tenderness in soft tissues
- Do lying and standing blood pressures
b. Identify any treatable/management areas e.g.
- Formal sleep disorders (obstructive sleep apnoea, restless legs, periodic limb movement disorder (PLMD))
- Inflammatory or degenerative arthritic conditions
- Other chronic conditions
- Depression or anxiety
- Irritable bowel syndrome
- Other primary pain conditions (headaches, pelvic pain, temporo-mandibular disorders, vulvodynia, etc.)
3. Investigations
Consider blood tests to exclude other conditions and identify treatable comorbidities
- FBC, CRP, ferritin, creatinine
- Electrolytes, renal and liver function, calcium, magnesium
- Fasting blood glucose and insulin
- Thyroid function and antibodies (TSH, T3, T4)
- B12, Folate, Vitamin D
- Iron Studies
- Urinalysis
- Coeliac antibodies
- Inflammatory muscle disease, creatinine kinase
- Immunoglobulins, antinuclear antibodies, rheumatoid titres
- Fasting am cortisol and DHEA
Other tests as clinically indicated:
- If associated with a viral illness, consider EBV, cytomegalovirus, HIV, QFever testing
4. Referral to Specialists as required
If there is significant uncertainty about the diagnosis, or predominant symptoms are suggestive of other underlying or overlapping diagnoses and for specific areas of management refer to specialists e.g. rheumatology, endocrinology, neurology, infectious disease, sleep, pain.
5. Further Assessment of Clinical Management Areas
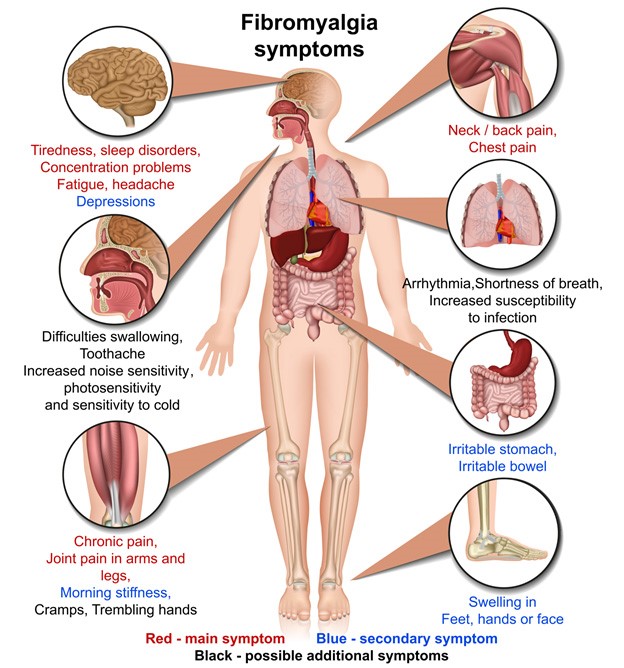
As fibromyalgia is not an exclusive diagnosis ask about other symptoms that may indicate overlapping and co-existing conditions e.g.
- Previous medical history, especially any chronic conditions e.g. headaches, anxiety, depression, back or joint pains
- Inflammatory arthritic conditions
- Medications (including over the counter), alcohol, and illicit drugs
- Weight loss, night sweats, psychiatric history, abuse, snoring
5.1 Pain or weakness
- Ask about:
- Pain in the muscles, joints, or both
- Widespread and migratory pain
- Significant headaches of new type, pattern and severity
- Ataxia, muscle weakness and fasciculations
5.2 Sleep dysfunction
- Unrefreshing sleep
- Disturbances in sleep quantity or rhythm, e.g. reversed or chaotic diurnal sleep rhythms
5.3 Fatigue
- The patient experiences significant physical and/or mental fatigue that substantially reduces their activity level and is:
- New
- Unexplained
- Persistent
- Recurrent
5.4 Gastrointestinal/Irritable bowel
- Constipation
- Diarrhoea
- Bloating
- Heartburn
- Abdominal pain or cramps
- Loss of appetite
- Vomiting
- Nausea
5.5 Neurological or cognitive symptoms
- Confusion
- Impaired concentration and short-term memory consolidation
- Disorientation
- Difficulty with information processing, categorising and word retrieval
- Perceptual and sensory disturbances e.g. spatial instability and disorientation and inability to focus vision
- Overload phenomena:
- Cognitive, sensory e.g. photophobia, hypersensitivity to noise
- Emotional overload – may lead to “crash” periods and anxiety
6. Other key symptoms requiring management
O Autonomic:
- Orthostatic intolerance – neurally mediated hypotension (NMH)
- Postural orthostatic tachycardia syndrome (POTS), delayed postural hypotension, light-headedness, extreme pallor, nausea and irritable bowel syndrome, urinary frequency and bladder dysfunction, palpitations with or without cardiac arrhythmia, exertional dyspnoea
O Neuroendocrine:
- Loss of thermostatic stability – subnormal body temperature and marked diurnal fluctuation, sweating episodes, recurrent feelings of feverishness and cold extremities, intolerance of extremes of heat and cold
- Marked weight change – anorexia or abnormal appetite, loss of adaptability, and worsening of symptoms with stress
O Immune:
- Tender lymph nodes, recurrent sore throat, recurrent flu-like symptoms, general malaise, new sensitivities to food, medications, or chemicals
- Does the patient have a history of post viral or ongoing infections that could be driving the symptom patterns?
7. Useful Assessment Tools to aid Diagnosis